Though more than two million people in the US are HIV positive — with more cases diagnosed each year — the human immunodeficiency virus no longer grabs headlines. A pill that helps prevent HIV isn’t grabbing headlines either. The Centers for Disease Control (CDC) wants to spread the word about this pill, an oral preexposure prophylaxis known as PrEP, but figuring out the best way to reach the target populations is a challenge.
Through a five-year CDC contract, UW professor Steve Goodreau and colleagues at Emory University are analyzing populations that would benefit from the medication and are predicting the pill’s potential impact based on a range of variables. They are now looking at the costs and benefits of approving PrEP for minors.
“PrEP is approved for use by adults 18 years or older,” explains Goodreau, associate professor of anthropology. “Prescribing PrEP for those under 18 is a big gray area right now, and few providers are willing to do it. But by the time they turn 18, somewhere around seven to ten percent of gay and bisexual males will be HIV positive, at least in some cities. Waiting until they are 18 is too late for a lot of kids. The CDC thinks it’s worth considering strengthening their recommendations around PrEP and adolescents, but before they go ahead with that, they want as much evidence as possible that it would be worth doing so. They know there will be pushback, since it raises a lot of sensitive issues.”

Those issues have come up before, with the introduction of the HPV vaccine, which prevents a virus that can cause cervical cancer and other health problems. The HPV vaccine works best if taken before an adolescent becomes sexually active, but many parents have balked at scheduling the vaccine, not wanting to think about their child having sex. And some sexually active girls have wanted the vaccine but were unwilling to tell their parents, raising the thorny issue of parental consent.
PrEP raises the same issues, with added complications. Unlike the HPV vaccine, which involves a series of three shots, PrEP must be taken on an ongoing basis. And the young people needing it most would be male adolescents having sex with other males. “That’s an additional discomfort that parents might not want to think about, or know about, or realize applies to their child,” says Goodreau. “But with a considerable number of teenage males getting HIV by the time they are 18, we have to think about it, whether we want to or not.”
By the time they turn 18, somewhere around seven to ten percent of gay and bisexual males will be HIV positive, at least in some cities. Waiting until they are 18 is too late for a lot of kids.
There are other tools for preventing HIV, most notably the condom. But, says Goodreau, “the fact that we still have unwanted pregnancies and we still have HIV transmission means that condoms don’t work for everyone all the time. PrEP is another tool in the toolkit. Taken daily, it can almost entirely prevent someone from getting HIV. Nothing is certain, but this is pretty close.”
Goodreau uses computer models to predict the impact of adolescents using PrEP and the optimal point for introducing the medication. “Is it worth trying to reach teens before they are sexually active, knowing that would be more difficult but would provide maximum protection?” asks Goodreau. “If we don’t get to teens until six months after they sexually debut, is that too late or does it still give us most of the benefits? Those are the kinds of things we’re looking at.”
In his computer models, Goodreau considers factors like age, onset of sexual activity, sexual networks, number of sexual partners, and openness to regular HIV testing. He uses data from existing surveys, including a nationwide online survey for men who have sex with men, and an annual health survey of high school students that covers sexual behavior, alcohol and drug use, exercise, diet, and more. Goodreau also uses data from an ongoing PrEP trial, including information about adolescents’ willingness to start PrEP and stay on it.
The models give the CDC a better sense of how many cases of HIV would likely be prevented, and at what cost, with different guidelines. The findings could lead to targeted outreach to teens, a revision in guidelines for doctors prescribing PrEP to teens, and other changes. For Goodreau, knowing that his work may have an impact on health policy is motivating.
“Modelling is good at asking, ‘If you could do X, what would the impact be?’” he says. “Some reseachers model things that are completely impossible, but I’m not interested in working on a project where X is completely impossible. As a social scientist, I always want to work on things that can be implemented. This PrEP study is a great example of that.”
More Stories

AI in the Classroom? For Faculty, It's Complicated
Three College of Arts & Sciences professors discuss the impact of AI on their teaching and on student learning. The consensus? It’s complicated.

A Sports Obsession Inspires a Career
Thuc Nhi Nguyen got her start the UW Daily. Now she's a sports reporter for Los Angeles Times, writing about the Lakers and the Olympics.
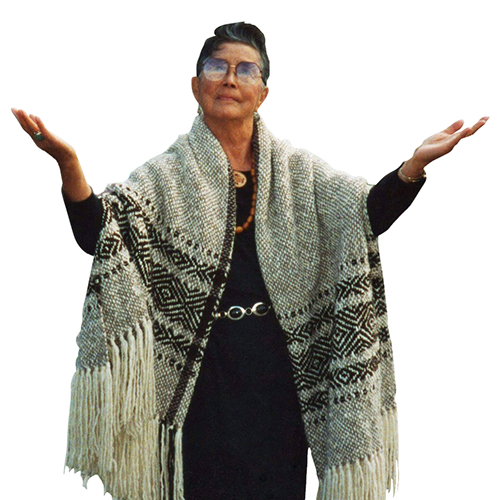
A Healing Heart Returns
In February, the UW Symphony will perform a symphony that Coast Salish elder Vi Hilbert commissioned years ago to heal the world after the heartbreak of 9/11. The symphony was first performed by the Seattle Symphony in 2006.